Pain relief and fever management are common concerns for many people. Tylenol, a well-known medication worldwide, has recently become the subject of intense debate. Former U.S. President Donald Trump made statements linking its use during pregnancy to autism, creating panic among medical experts and confusion among expectant mothers.
Pregnant women, parents, and health advocates have relied on Tylenol to relieve headaches, body pain, and fever for years. At the same time, researchers continue to investigate potential connections between acetaminophen (also known as paracetamol) and neurodevelopmental outcomes, including autism.
This blog will explore what Tylenol is, its ingredients, and its effects on pregnancy and autism. We will also examine the current debates and the findings of scientific studies.
Our goal is to present a clear, evidence-based perspective rather than sensational headlines so that readers can make informed choices in consultation with their healthcare providers.
Key Takeaways:
- Acetaminophen is the active ingredient in Tylenol, also known as paracetamol in other regions.
- Pregnant women commonly use it to manage fever and pain during pregnancy. It is considered a safe medication.
- Donald Trump’s recent statements about Tylenol’s effects on autism and pregnancy have faced widespread criticism from medical experts and health agencies, who deem them misleading.
- An untreated fever can pose risks for expectant mothers, so avoiding essential safe medications is not advisable.
- Always consult your healthcare professional before believing any claims regarding health and medications.
Table of Contents
What is Tylenol, and What Is It Used For?
Acetaminophen, also known as paracetamol or Tylenol, is a non-opioid pain reliever and fever reducer. It is an active ingredient in many prescription medications and is used to treat various conditions such as:
- Mild to moderate pain from headaches
- Muscle aches
- Toothaches
- Menstrual cramps
- Colds
- Sore throats
- Reactions to vaccinations
- Osteoarthritis pain
- Reduce fevers.
Tylenol is commonly found in cold, flu, and multi-symptom medications. However, caution is essential to prevent overdosing when using multiple products. Its primary benefits are pain relief and reducing fever. Be aware that an overdose can result in serious liver damage or failure.
Ingredients in Tylenol

The active ingredient in Tylenol is acetaminophen, which is also known internationally as paracetamol. Its chemical name is N-acetyl-para-aminophenol (commonly abbreviated as APAP). In addition to the active drug, Tylenol formulations often contain excipients, such as fillers, binders, coatings, dyes, and preservatives, which vary depending on the form (tablet, liquid, capsule). Some formulations may also include additional agents, such as those found in extended-release forms or combination products. However, the primary effects of pain relief and fever reduction are attributed to acetaminophen.
Acetaminophen vs Paracetamol- Are They the Same?
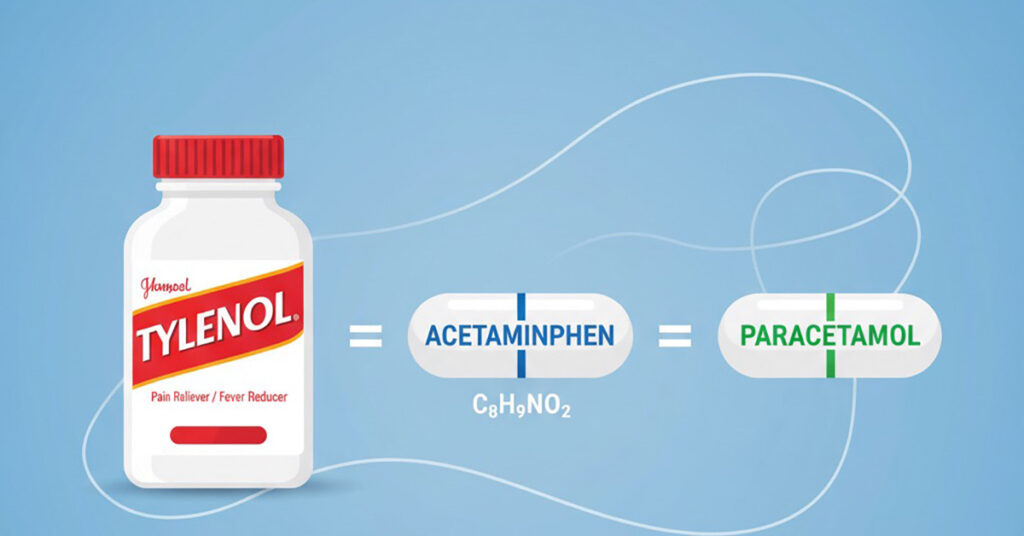
The terms “acetaminophen” and “paracetamol” refer to the same molecule and have the same functions and metabolism. The distinction between the two names is primarily based on regional naming conventions. In the United States and parts of North America, “acetaminophen” is the standard term used, while in the UK, Europe, India, Australia, and many other regions, “paracetamol” is the more common name. In short: Tylenol = acetaminophen paracetamol.
The Controversy Surrounding Trump’s Claim

Claims from the Trump White House regarding a potential link between the use of the painkiller acetaminophen commonly known by the brand name Tylenol in the U.S. during pregnancy and the development of autism have sparked significant responses from the medical, scientific, and public health communities. On September 22, 2025, Donald Trump, accompanied by HHS Secretary Robert F. Kennedy Jr. and Dr Mehmet Oz, publicly declared that Tylenol (acetaminophen) use during pregnancy is linked to autism in children. He suggested that groups such as the Amish or Cubans, who allegedly do not use Tylenol, have lower rates of autism. In a White House statement titled “FACT: Evidence Suggests Link Between Acetaminophen and Autism,” his administration framed this claim as part of a new initiative for health guidance.
Autism and Tylenol: Causes & Risk Factors
To understand the claims linking Tylenol to autism, it is important to distinguish between what is established and what is speculative regarding the origins of autism. Autism Spectrum Disorder (ASD) is a complex neurodevelopmental condition characterized by differences in social communication, behavior, and sensory processing. Genetic factors play a significant role, as numerous studies have shown a high heritability rate, the involvement of multiple genes, and the presence of de new mutations in some cases. In addition to genetic influences, environmental or non-genetic factors are believed to modulate the risk of developing ASD. These factors may include prenatal exposures, maternal health, infections, inflammation, exposure to certain chemicals, maternal metabolic conditions, and more.
Does Tylenol Affect Pregnancy?

Most medical organizations consider acetaminophen to be one of the safest options for pregnant women when taken at the lowest effective dose for the shortest duration necessary. Not treating a high fever during pregnancy can lead to risks such as neural tube defects, miscarriage, and preterm birth. While “safe” does not mean “risk-free,” acetaminophen remains a primary choice compared to other options. Overdose is always a concern; acetaminophen overdose is one of the leading causes of acute liver failure.
Making informed choices during pregnancy is a key part of overall women’s health, especially when it comes to medications. Understanding what is safe and what is not must be based on evidence and not based on any random information.
WHO’s Statement
On September 24, 2025, the World Health Organization (WHO) released a statement addressing claims that using acetaminophen during pregnancy is linked to autism. The WHO emphasized that there is no conclusive scientific evidence supporting this connection. Despite extensive research, studies have not consistently shown a link between prenatal acetaminophen use and autism.
The World Health Organization (WHO) has emphasized that autism is a complex neurodevelopmental condition influenced by many interacting factors. The exact causes of autism are still unclear, and no single factor, including acetaminophen, has been proven to be responsible for its development.
WHO advises pregnant women to use medications cautiously, particularly during the first trimester, and always under the guidance of a doctor or qualified health professional. While acetaminophen is generally considered safe for short-term use, it should only be taken when necessary and with medical oversight.
Finally, the WHO called for continued research into the causes of autism and urged global efforts to improve care and support for autistic individuals and their families. The organization highlighted the importance of understanding autism through evidence-based approaches, free from stigma.
Statements from Other Expert Institutions
- EMA’s Chief Medical Officer, Steffen Thirstrup:
“Paracetamol remains an important option to treat pain or fever in pregnant women. Our advice is based on a rigorous assessment of the available scientific data and we have found no evidence that taking paracetamol during pregnancy causes autism in children.”
- Steven J. Fleischman, MD, MBA, FACOG, president of the American College of Obstetricians and Gynaecologists (ACOG):
“Suggestions that acetaminophen use in pregnancy causes autism are not only highly concerning to clinicians but also irresponsible when considering the harmful and confusing message they send to pregnant patients, including those who may need to rely on this beneficial medicine during pregnancy.
“Today’s announcement by HHS is not backed by the full body of scientific evidence and dangerously simplifies the many and complex causes of neurologic challenges in children. It is highly unsettling that our federal health agencies are willing to make an announcement that will affect the health and well-being of millions of people without the backing of reliable data”
- Society for Maternal-Fetal Medicine (SMFM):
In response to today’s White House press conference announcement, the Society for Maternal-Fetal Medicine (SMFM) reiterates its recommendation advising both physicians and patients that acetaminophen is an appropriate medication to treat pain and fever during pregnancy.
Despite assertions to the contrary, a thorough review of existing research suggesting a potential link between acetaminophen use during pregnancy and an increased risk of autism and attention-deficit hyperactivity disorder (ADHD) in children has not established a causal relationship.
Conclusion
Tylenol has been trusted for decades as a safe and effective pain and fever reliever, even during pregnancy. Although there is a growing public debate linking autism to Tylenol, scientific evidence does not support any causal connection between the two. Claims made by Trump suggesting that Tylenol causes autism have been widely discredited by experts. The real danger lies not in the responsible use of acetaminophen, but in the misinformation that may discourage pregnant women from treating serious conditions like fever. It is crucial to be well-informed before trusting and acting on any information.
Frequently Asked Questions
1. How long does Tylenol stay in your system?
A typical dose of Tylenol begins to leave the body a few hours after ingestion, which is why its effects may wear off in four to six hours. However, complete clearance of acetaminophen from the body can take up to 24 hours. This duration may vary based on factors such as the dose taken, liver function, age, and overall health.
2. Why does pain get worse at night?
Several factors can contribute to an increased perception of pain, including reduced activity levels, changes in posture, decreased distractions, fluctuations in hormone levels, and sleep disturbances. When we are tired, the brain struggles to regulate pain signals, known as anti-nociceptive pathways, resulting in a heightened perception of pain.
3. Is CROcin a painkiller?
CROcin is a powerful painkiller specifically designed to alleviate headaches. It works by inhibiting the chemical messengers in the brain that transmit signals related to pain and discomfort. By blocking these signals, CROcin effectively disrupts the headache cycle, providing relief and restoring a sense of comfort to those who suffer from this common ailment.
4. Which painkiller makes you sleepy?
Opioid medications, including hydrocodone/acetaminophen (commonly known as Norco), oxycodone (available as Roxicodone or OxyContin), and acetaminophen/codeine (referred to as Tylenol #3), are primarily prescribed for pain management. These medications are known for their potent analgesic effects, but they also carry a risk of significant sedation
5. Is Tylenol a blood thinner?
Tylenol is not a blood thinner. Blood thinners are medications that help blood flow more easily through your arteries and veins. It is generally safe to take Tylenol while using blood thinners. However, be cautious about overdosing, as it can cause liver damage.